Scaling Compassion: How Pacific Clinics Transformed Access to Behavioral Health With Agentforce
Case Study Overview
Pacific Clinics is California’s largest community-based provider of behavioral and mental health services.
Following a merger, the organization now has over 2,200 employees who help deliver programs and services to more than 100,000 people annually. It was a huge opportunity for Pacific Clinics to boost its impact. However, it required a seismic technology transformation to build something new, intentional, and ready for the future, so they could spend more time delivering trauma-informed care that doesn’t just change lives, but saves them too.
But at the time of the merger, their systems were not optimized for the organization’s expanding scale. Demand for services was rising, and employees were spending countless hours on manual tasks that had the opportunity for automation. At the same time, the behavioral health sector was facing a long-term workforce shortage that, according to CEO/President Kathy McCarthy, is unlikely to be resolved in the near future.
As she has emphasized, this ongoing challenge makes it critical to use technology to extend employee capacity while maintaining quality and sustainability. And with CalAIM opening the door for true client choice, allowing individuals to reach out directly to Pacific Clinics for care and vice versa, it needed systems that could facilitate this transformative new model of client engagement and outreach at scale.
This tumultuous environment drove Pacific Clinics to partner with Provisio to build a technology foundation that unifies data, automates processes, modernizes client access, and builds a long-term architecture for sustainable growth through AI-supported adoption.
These solutions span:
Enhanced Care Management outreach under CalAIM
Mobile crisis response and call center operations
A unified data and automation layer
Agentic AI with Agentforce, to assist with client engagement and employees
The result: a human-centered technology transformation that enables internal teams to focus on what matters most: providing compassionate, high-quality care.
The Challenges
A tidal wave of data, but no unified way to act on it
For CalAIM’s Enhanced Care Management program, Pacific Clinics receives thousands of contacts from health plans via spreadsheets. For just one plan, employees spent 80 hours per month manually:
Downloading and parsing files
Identifying new members and updating information
Entering data into their EHR
Reconciling billing details
Each plan had its own file format and often outdated information, so employees were buried in spreadsheets instead of engaging clients.
Crisis response built on chat, texts, and guesswork
Before November 2022, the Pacific Clinics crisis team delivered high-quality service through proven programs, but without a fully centralized technology platform to support increasing demand, such as:
No single technological system to manage mobile responses
Incoming calls were routed to individual desk phones, limiting shared visibility and flexible call handling
Dispatch coordinated relied on Microsoft Teams messages, texts, and emails
Reporting required manual review of phone logs, making real-time insights difficult
As call volume grew, response times at times approached an hour, and leadership lacked real-time visibility into call volume, call types, and team assignments. These challenges reflected not the program's quality but systems that had not yet evolved to match the team’s scale, creating a clear opportunity for AI-supported coordination, automation, and real-time insights.
A sector shift toward client choice and direct access
Under California’s evolving CalAIM model, Pacific Clinics is moving from a system where counties assign clients to one where clients can reach out directly and exercise real choice. That shift toward client choice raised hard questions:
How do we handle thousands of referrals per week quickly and consistently?
How do we ensure the right clients reach the right programs sooner?
How do we provide high-quality service to potential clients if employees are overwhelmed by the volume?
How do we support employees who are stretched thin?
Due to an industry-wide worker shortage, technology had to help stretch resources without compromising care or safety.
Fragmented systems, fragmented view
Across a wide array of programs, Pacific Clinics managed different workflows, data, compliance rules, and funding sources.
Leaders couldn’t easily view a comprehensive funding portfolio for a given program, identify service gaps, or quickly retrieve outcome data for funders or for new opportunities. Due to its size and scale, it became necessary to track funding and programming simultaneously.
AI opportunity, but real risks for vulnerable populations
Pacific Clinics has been talking about how to use technology with vulnerable populations safely:
How to prioritize human connection to deliver compassionate care
How to use digital tools to help people take a first step
How to avoid exposing clients to unsafe experiences
It was clear to Pacific Clinics they needed responsible data practices, clear guardrails, and a focus on assisting employees – not replacing them.
The Solutions
From 80 hours of manual work to automation
Enhanced Care Management (ECM)
MuleSoft integration to consume health plan files and transform data into consistent values
Automated loading of transformed data into Service Cloud
Creation of new patient records in their EHR and consolidation of billing information
Integrated outreach via Service Cloud + Salesforce Voice + Amazon Connect, so the team can manage and track outbound calls from a single place
What used to take weeks of manual entry is now an automated process.
TRUST: A new model for crisis response in Santa Clara County
Community crisis & mobile response
Santa Clara County wanted a way to respond to certain community crises without involving law enforcement. Pacific Clinics, already the county’s primary mobile crisis partner, engaged local community partners to launch the county’s TRUST Program (Trusted Response Urgent Support Team).
Provisio helped design and implement a Salesforce-based solution that now powers this community-driven model:
Call handling & real-time field updates on Salesforce
Employees are trained to receive calls directly on their computers, guided through a responsive screening process that gathers essential details. Field Service–powered dispatch displays all response vans on a map, allowing employees to dispatch the nearest team based on location and availability.
Both callers and responders receive real-time updates: responders get all information on their mobile devices, while callers receive a text with a map link showing the team's exact location. Additional texts inform callers about the team's proximity and estimated arrival time. Leadership benefits from live, actionable data through dashboards that display call volume and types, offering insights to improve the program.
Becoming an agentic nonprofit with Agentforce
Pacific Clinics became one of the first nonprofits to implement Agentforce, supporting their rapidly growing caseloads. After years of groundwork on data, processes, and innovation, they were ready to adopt agentic AI in ways that directly serve clients and employees. Together, Provisio and Pacific Clinics implemented two core agents:
HOPE Benefits Agent: A compassionate, client-facing agent
A 24/7 client-facing agent named HOPE integrated into Pacific Clinics’ Enhanced Care Management program helps potential and current clients by providing information about ECM, checking eligibility, and answering program-related questions around the clock.
The agent facilitates early connection to health and support services as clients show interest, schedules callback times for employees, and highlights urgent needs for prioritization.
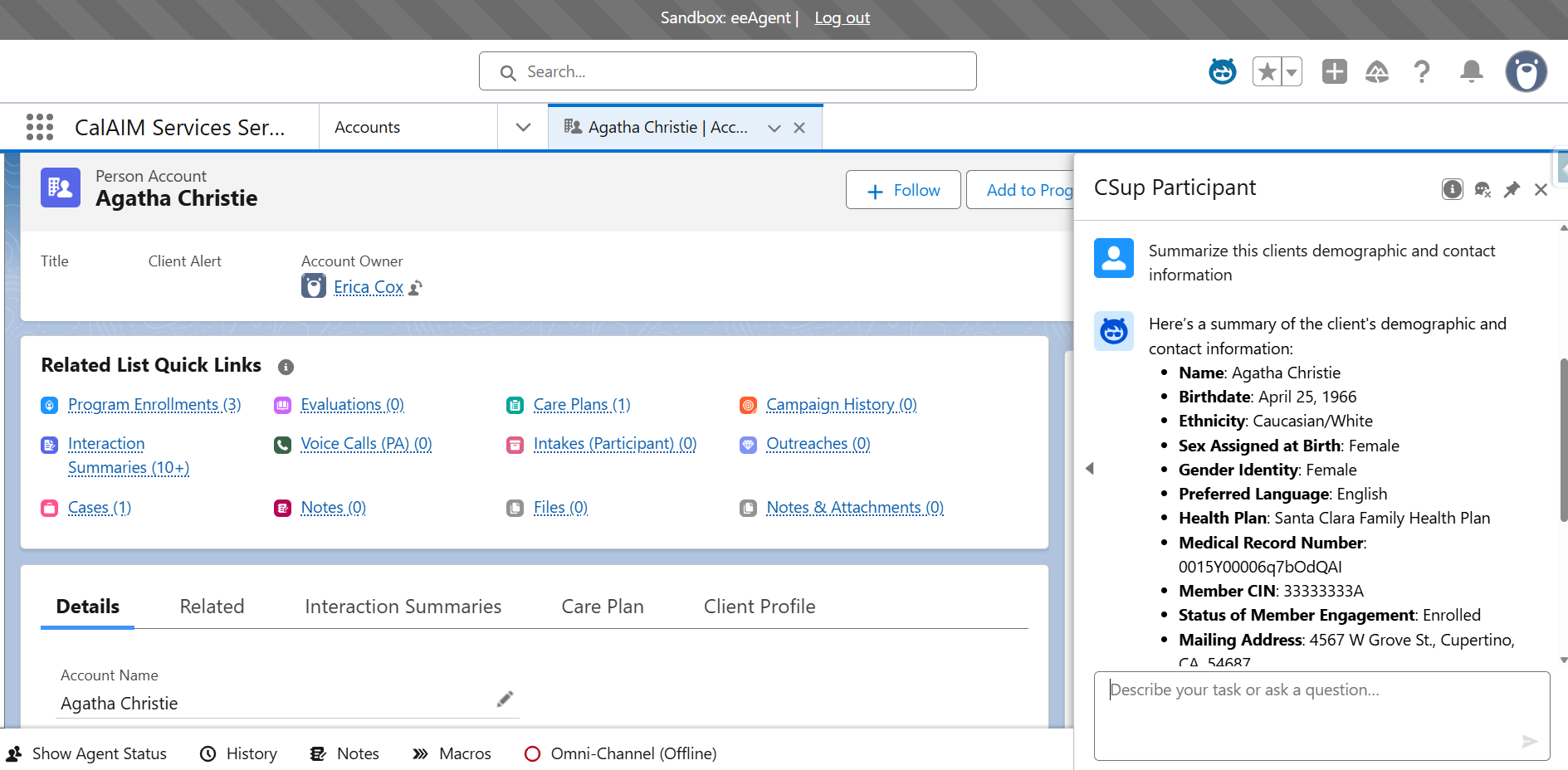
Participant Management Agent: Giving Pacific Clinics a real-time, 360° view
An employee-facing agent that quickly summarizes a client’s information in real time. Pulls together data from across 200+ programs, each with its own workflows and compliance rules. Their team can immediately view the programs the client is enrolled in, their progress in the care plan, and the current status of services.
Employees can ask the agent to summarize the client, log today’s call, note that it has been reviewed, and update records without having to click through multiple screens.
Using agents to support strategic decisions, not just transactions
Because funding, program data, and client outcomes now live in a unified environment, leaders can use the agents to:
See complete funding portfolios for a program
Match activities and services to specific funders in near real time
Identify service gaps across programs and geographies
Hand curated insights directly to apply for contract expansions and grants
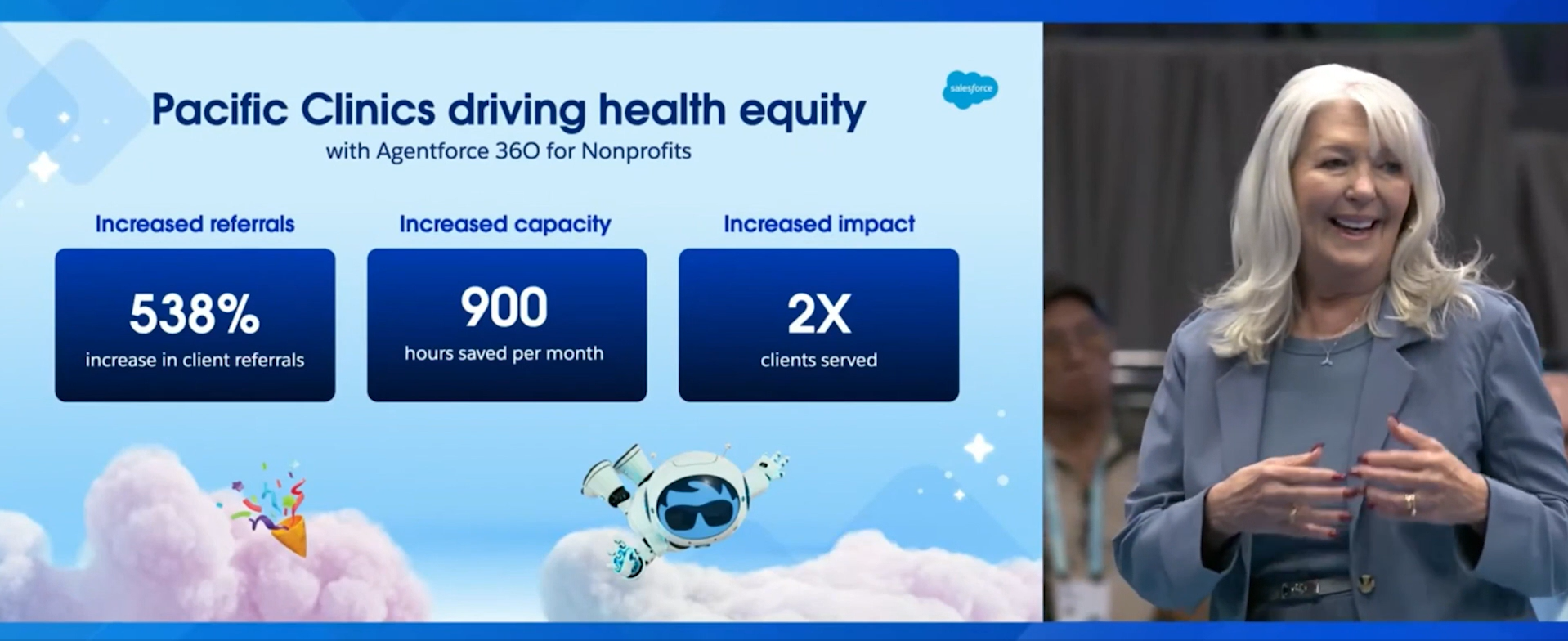
Tangible Outcomes
Across ECM, crisis response, and AI adoption, Pacific Clinics is seeing measurable impact.
Access to care & referrals
538% increase in access to referrals
2× as many clients served in just 12 months
Faster response & improved experience
Response times decreased from 50–60 to 15–30 minutes
Callers get real-time updates by text and see team location on a map.
Employee time & capacity
~900 hours per month saved by eliminating manual data entry
Processing dropped from 80 hours to 15 minutes per month
“We are going to enhance and augment the services with technology to take as much of the administrative burden, repetition, agonizing, time-wasting activity—and do as much as we can to ensure employees are focusing on why they came to work in this field, which is to serve people.”
Kathy McCarthy, CEO & President at Pacific Clinics
A model for how human services organizations can scale impact when technology is designed with people at the center.
Pacific Clinics has always centered its work on measurable outcomes, and their expansion further aligned their technology investments to scale services and improve results. Provisio brought the technical and human services expertise, together with Salesforce, to turn that vision into a practical digital workforce that can ethically and responsibly enhance its team with AI-driven technology.
This partnership is a blueprint for what’s possible when technology transformations are human-centered and rooted in an organization’s mission.